This podcast delves into the fundamentals of bariatric surgery, exploring four major procedures—gastric band, sleeve gastrectomy, Roux-en-Y gastric bypass, and duodenal switch. Learn about patient considerations, surgical impacts, and the importance of postoperative care for long-term success.
Transcript
[00:00] Hello and welcome back once again to Surgery 101, the podcast series brought to you with the help of the Department of Surgery at the University of Alberta. This is Jonathan White broadcasting to you
[00:20] live from the Royal Alexandra Hospital in Edmonton, Alberta. This week’s episode is number 3 in a series on bariatric surgery and obesity, brought to us by medical student Julie La, who is visiting on a surgical educational active from McMaster University. In this episode, Julie will be getting to the main topic, the bariatric surgery
[00:40] itself she’ll be giving a brief overview of the four main procedures, the gastric band, the gastric bypass, the sleeve gastrectomy and the juillenal switch. So let’s get ready to get all the way up into bariatric surgery itself here on surgery 101.
[01:00] Hi everyone, my name is Julie Law and I’m a third and final year medical agent.
[01:20] Student at McMaster University in Hamilton, Ontario. This podcast was written and produced with guidance and support from Jenny Marshall, program assistant in digital education, and Dr. Jonathan White, general surgeon at the University of Alberta, creator of Surgery 101. The expert content reviewers were Dr. Alia Kanji, bariatric surgeon at the University of Alberta, and Dr. Renika Moti,
[01:40] assistant clinical professor in the Department of Family Medicine at the University of Alberta, and medical lead for the Edmonton Adult Bariatric Clinic. The topic of today’s podcast is surgical options for the management of obesity. By the end of this episode, you should be able to describe various types of bariatric surgery, including the adjustable gastric band,
[02:00] sleeve gastrectomy, row and wide gastric bypass, and the duodenal switch. Let’s start by reviewing the NIH
[02:20] guidelines for bariatric surgery. 1. Age 18 to 64 2. BMI greater than 40 or BMI greater than 35 with comorbidities such as type 2 diabetes, cardiovascular heart disease, severe obstructive sleep apnea, or GERD. 3. Some contraindications include current
[02:40] substance dependency, recent major cancer, untreated psychiatric illness, diseases that would make you ineligible for any surgery, if you are pregnant, have cirrhosis, or chronic pancreatitis. Most bariatric surgery is performed by general surgeons with subspecialty training in minimally invasive surgery and bariatrics.
[03:00] Bariatric surgery has been evolving since the 1950s. Many groups around the world recognized obesity as a medical issue and began to try various ways to reduce the size of the stomach, the concept of restrictive surgery, rearrange the intestines to facilitate malabsorption, and then eventually a combination of both. As we learn more about
[03:20] how and why bariatric surgery works, we are learning that there are a number of gut hormones that are involved in augmenting weight loss in these procedures. These procedures, while initially done open, are now almost exclusively performed laparoscopically. In Canada, bariatric surgery is covered by our Public Health Plan, which is decided upon provincially.
[03:40] With that, there is variation in procedures that are covered. In Ontario, where I’m from, the Ministry of Health funds three types of bariatric surgery, all of which are done laparoscopically. The Roux-en-Y gastric bypass, the vertical sleeve gastrectomy, and the duodenal switch. In Alberta, the duodenal switch is not yet performed, but the adjustable gastric bandage.
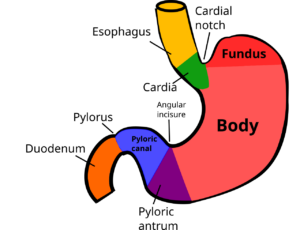
[04:00] is. Now to review the steps in anatomy of bariatric surgery. These can be tricky to follow. Honestly, reading them in textbooks repeatedly was even difficult to follow. I hope that I’ve simplified things and the slides that we provided will be a helpful tool. This might be a section that needs a few listens.
[04:20] The first procedure I’ll discuss is the adjustable gastric band. The gastric band was initially approved by the FDA in 2000. Since then, hundreds of thousands of these bands were placed around the world. The principle behind this procedure is the placement of a foreign body, the adjustable gastric band around the proximal
[04:40] stomach. This is then connected via tubing to a port that sits on the fascia below the skin. The port can then be accessed to inflate the band with saline or deflate the band removing saline. The adjustment is to allow for more or less restriction. The band was initially a very attractive weight loss procedure as it is minimally invasive, adjustable, and
[05:00] completely reversible. Unfortunately with it were many complications that led to a large number of these bands being removed. Next the components of the Roux-en-Y gastric bypass. This procedure includes the pouch,
[05:20] which is a small segment of the stomach that is stapled off. It acts as the new gastric reservoir with a much smaller volume. This will help decrease overall intake and increase the sense of satiety or fullness. Next is the bypass part, where a distal portion of the small intestine, the jejunum, is divided and then attached to the gastric pressure.
[05:40] pouch. This is called a gastrostomach to jejunum jejunostomy. This is the new pathway that food will travel and it’s called the Roo Lim. Recall the physiology of obesity. One simple way to look at it is energy in versus energy out. Using a distal portion of the small intestine will
[06:00] result in bypassing a large absorptial surface, decreasing the amount of energy in. Okay, now about 100 to 150 cm downstream from this new connection, the proximal aspect of the jejunum from your division is connected to a downstream part of your small intestine. Remember, this connection goes
[06:20] from the bottom part of your stomach, the distal stomach, from where the pouch was stapled off, all the way down to the proximal jejunum. But as you might notice, there’s an important area stuck between the stomach and the jejunum, the duodenum. This area contains the outlet for digestive enzymes and bile to drain. This anastomosis is
[06:40] called an enteroantorastomy, and it is to allow for pancreatic and biliary secretions to mix with ingested food much later in the GI tract, enhancing the restriction of the energy that’s absorbed. A vertical sleeve gastrectomy
[07:00] is much simpler than a Roux-en-Y gastric bypass. This will be a break in our podcast. It involves removing a large portion of the stomach, leaving the lower esophageal sphincter and pylori intact. You’re left with the stomach roughly shaped like a banana. With the sleeve, there is lower morbidity and mortality, given that the small intestine is not involved.
[07:20] Finally, we have the newest surgical procedure, the duodenal switch. This is also known as the biliopancreatic diversion with duodenal switch. This one can be the trickiest to follow, so I’d recommend following along with the drawing.
[07:40] The first step of this procedure is the vertical sleeve gastrectomy. Again, this procedure results in a banana-shaped stomach. After this is the duodenal cut or transection proximally before the ampulla where the bile and digestive juices will drain. So next is the duodenal switch part of the surgery. To make a new path for ingested food, there is a roux limb form.
[08:00] formed with an ileal transection that is about 250 cm from the ileocecal valve and the ileum is connected to the proximal duodenum, a duodenum ileostomy. Let’s think about this for a second. Food goes into your mouth, down the esophagus, into the sleeve, the banana-shaped stomach, exits
[08:20] and enters the proximal duodenum before any pancreatic or biliary digestive juices have made contact. Then it passes the new connection, the duodenal ileostomy, and whoa, it’s now in the ileum, completely bypassing most of the duodenum, the jejunum, and some ileum, the absorptive surface that it’s missed. And this helps a lot with restricting energy uptake.
[08:40] Let’s get back to the procedure, the other half of the duodenal switch, which involves the other part of the duodenum, the distal aspect, which still has the ampulla for drainage of bile and pancreatic digestive enzymes. This is connected to the ilium, which is quite far downstream. Let’s think, why would we do this? Well, this length of bowel contains all the drainage from the big
[09:00] biliary tract and pancreas. Of course, as you know, digestive enzymes and bile are essential in breaking down and absorbing nutrients. Basically, in the bariatric population, it is a fine balance between restriction for weight loss and sufficient absorption to prevent malnutrition.
[09:20] Now that we’ve discussed four different types of bariatric procedures, let’s compare the options why one surgery may be chosen over another. As you can see moving from left to right on the chart, the more involved and complex the surgery is, the more success with weight loss can be achieved. However, there’s a higher incidence
[09:40] of complications. Choosing which surgery is right for each person involves a careful discussion with the patient and the surgeon. Taking into consideration factors such as patient, age, comorbidities, desired weight loss and patient preference is important. Now that we’ve reviewed the various weight loss procedures, impact on comorbidities, and weight loss expectations,
[10:00] patients, it is important to once again recognize that bariatric surgery is a tool for patients with obesity. The postoperative care which involves maintaining a detailed food diary, regular follow-up with a dietitian, ongoing cognitive behavioral therapy to manage previous maladaptive eating behaviors, and engaging in regular physical activity
[10:20] are key to weight loss maintenance and success after surgery. Thank you so much for listening to the third podcast in our series of five on obesity medicine and bariatric surgery. Hopefully you are now familiar with what bariatric procedures exist and the fundamental concepts behind them. I’m looking forward to our final two podcasts on the flow of a bariatric patient from
[10:40] community to surgery and to review the complications of the bariatric surgeries. Thanks Julie for this great overview of the techniques involved in
[11:00] bariatric surgery. Please let us know what you think of this episode and all of our episodes. You can contact us through surgerypodcastsatgmino.com or find us on Twitter, surgeryunderstore101 or just drop into the website, surgery101.org and contact us that way. Thanks for listening and we’ll see you back here next week
[11:20] for a little bit more bariatrics on surgery 101.